Do you turn to alcohol to cope with feelings of depression? Maybe you drink to forget about a painful breakup or to relieve the stress of your job. While alcohol may provide temporary relief, it can lead to a dangerous cycle of using alcohol to manage negative emotions. Research shows that people struggling with alcohol use disorder (AUD) are three times more likely to experience major depression. This connection isn’t coincidental. Alcohol and depression often feed into each other, creating a destructive cycle that can be hard to break. Understanding depression, its various forms, and how it interacts with alcohol use is the first step toward breaking this cycle.
Like many mental disorders, various types of depression have different causes. Here are the most common types of depression and how they can appear:
Beyond these few, there are many other forms that depression can take and similar disorders that may look like depression on the surface. If you think you may be experiencing depression or a related condition, talk to your doctor and reach out to trusted people for help.
Symptoms may vary from person to person, depending on each individual’s circumstances. Not all symptoms may be present, and other symptoms not appearing on this list may be related to depression.
Some common symptoms associated with depression and related disorders are:
If you or a loved one has been experiencing one or more of these for a prolonged period (often at least two weeks) and/or they’re negatively impacting you at home, work, or school, talk to your doctor about the possibility of depression. Certain symptoms may be more severe than others, and a few carry a higher risk, especially relating to self-harm. Professional advice, particularly mental health care, should be sought immediately when thoughts of harm are involved.
Depression can affect anyone at any time, regardless of age, race, gender, income, or other demographic differences. There are, however, genetic, environmental, physiological, and other factors that increase an individual’s risk of developing depression. The factors that tend to most impact someone’s risk include:
Although there are clear risk factors for developing depression, no one knows exactly what causes it. One thing that psychologists do know is that biological differences in someone’s brain chemistry can play a large role in the development of depression and other mood disorders. Specifically, recent research indicates that changes in certain chemicals or neurotransmitters in the brain may contribute to someone’s risk of depression. Hormone changes in the body can also contribute to depression, as is often the case with postpartum depression. However, not everyone who has brain differences or hormonal changes develops depression, so these factors can’t be proven causes of the disorder.
Researchers also consider co-occurring disorders by studying the causes and risks of mental health conditions. Depression often occurs alongside another mental health disorder or medical problem. Those with existing mental health conditions like ADHD, PTSD, anxiety, and others are at a higher risk of developing depression, as are those with illnesses like cancer, multiple sclerosis, Parkinson’s, and more. Those with a dual diagnosis of two existing disorders need to address both issues in treatment to find long-term relief.
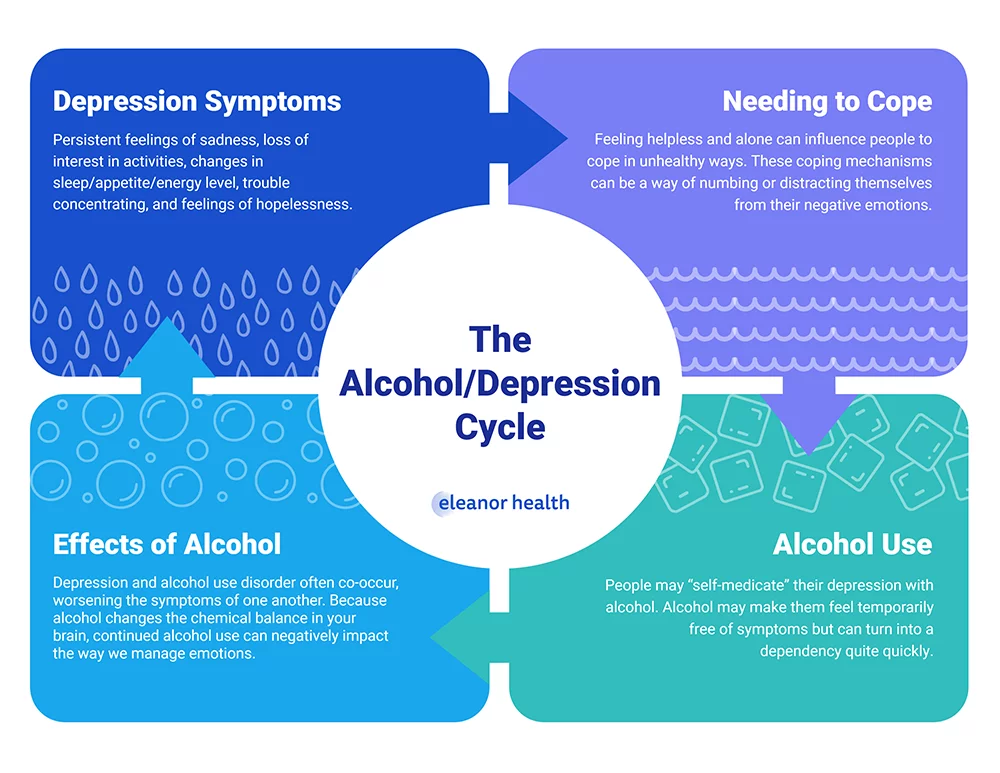
For people living with clinical depression, especially if it’s undiagnosed or untreated, drinking can feel like an escape. Using alcohol to numb sadness or loneliness may provide short-term relief, but it often creates a vicious cycle of negative emotions and dependency. In fact, more than 30% of people with alcohol use disorder experience this cycle firsthand.
The answer to both questions is “yes.” Research shows that people with depressive disorders often turn to alcohol as a way to cope with their symptoms. However, long-term alcohol use can lead to dependency and worsen depressive symptoms. Similarly, drinking can exacerbate depression symptoms because alcohol is a depressant that slows brain functioning and disrupts the balance of neurotransmitters responsible for managing emotions.
In fact, the connection between drinking and depression has become so significant that the DSM-5 now includes a new subsection of depressive disorders called “Substance/Medication-Induced Depressive Disorder.” This disorder is characterized by a prominent and persistent disturbance in mood caused by the use of substances and/or medications.
Breaking the cycle of alcohol use and depression requires commitment and support. Here are some tips to help you get started:
At Eleanor Health, we offer care and treatment that takes into account the whole individual, meaning that we focus on one’s life experiences, cultures, and values when offering assistance. With resources available in medication-assisted treatment, therapy & counseling, psychiatry, recovery coaching, and more, we are dedicated to helping you get to a place where you feel happy and healthy.
If you are seeking help with your loved one’s addiction, contact us today or complete our quick contact form below to speak with an addiction treatment specialist.
If you need help with your substance use disorder, we are here to help you build your confidence and momentum towards the future you want. We provide online treatment services for adults with alcohol, opioid, and other substance use disorders.
 Therapy for Anxiety, Depression, Trauma: 3 Common Types
Therapy for Anxiety, Depression, Trauma: 3 Common Types
 Mixing Lexapro and Alcohol: Side Effects and Risks
Mixing Lexapro and Alcohol: Side Effects and Risks
 The Link Between Anxiety and Alcohol
The Link Between Anxiety and Alcohol