Medications for addiction treatment (MAT) are increasingly utilized to combat the opioid crisis. The growing awareness of their use and effectiveness in addiction maintenance treatment has turned them into an important component to combat the alarming rate of opioid-related overdose and deaths. According to the United States Drug Enforcement Administration, over 64,000 died due to the use of synthetic opioids in a twelve-month period ending in January 2022.
MATs are used in different treatment stages and are usually complemented with behavioral therapies and counseling sessions to provide a more whole-person approach to treatment. And one of the medications utilized in opioid addiction treatment is Suboxone.
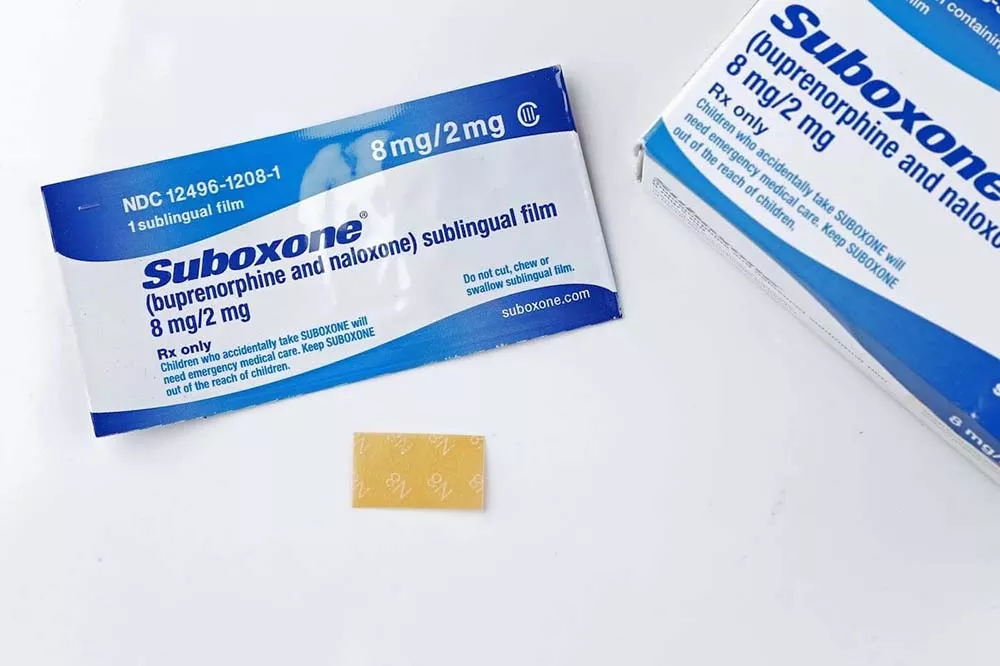
Suboxone is a prescription medication that contains buprenorphine and naloxone as its primary ingredients. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), buprenorphine is a partial opioid that blocks opioid receptors and decreases cravings. And the second active ingredient, naloxone, helps counteract the effects of opioids and minimize the risk of misuse. In addition, both compounds work together to eliminate the symptoms of withdrawal associated with opioid addiction.
Buprenorphine and naloxone are opioid-based medications that aren’t as addictive as heroin or prescription painkillers. Instead, Suboxone tricks the brain into thinking it’s getting the opioids it craves, and in turn, satisfying the physical dependence on opioids. This feature aids in the successful management of opioid withdrawal symptoms during recovery.
Suboxone for opioid addiction treatment is generally prescribed during the onset of acute opioid withdrawals to prevent the risk of precipitated withdrawals (the sudden occurrence of intense withdrawal symptoms). The duration of Suboxone treatment is determined by the specific needs and requirements of each individual. Suboxone maintenance programs provide a long-term treatment option for opioid use disorder.
The half-life of the opioid being misused determines when Suboxone treatment begins. For example, OxyContin and heroin have a short half-life and leave the body in a couple of hours. Suboxone is therefore prescribed at least 12 hours after the last dose of short-acting opiates and at least 24 hours after the last dose of long-acting opioids.
Suboxone is used in MAT treatment to help people wean off opioids and avoid inpatient detoxification. Suboxone’s key advantages are as follows:
While Suboxone is an effective MAT treatment, its prolonged use can lead to the development of dependence. In addition, Suboxone, as a partial opioid medication, can cause similar withdrawal symptoms to other opioids during abrupt cessation. Hence, individuals in Suboxone treatment are gradually tapered off the medication towards the end of their treatment to reduce the risk of Suboxone withdrawals.
Suboxone, like all opioids, can cause physical dependence when used for a prolonged period, even when taken as prescribed. Although the buprenorphine in Suboxone does not activate opioid receptors to the same extent as most potent opioid medications, it still blocks them to reduce cravings for other opioids. And as a result, cause withdrawal symptoms during abrupt cessation of Suboxone. This reaction is caused by the sudden absence of the medication, inducing a chemical imbalance in the body and triggering distressing effects. However, Suboxone withdrawal is relatively less intense than other opioid withdrawals.
Suboxone withdrawal symptoms include:
Individuals on Suboxone treatment should seek the advice of their treatment provider before quitting the medication. As abrupt cessation of Suboxone could lead to opioid withdrawal symptoms and increase the chances of a relapse.
Suboxone is a long-acting opioid with a half-life of 24-60 hours. Hence, symptoms of Suboxone withdrawal do not set in as quickly as other opioids, and withdrawals generally last longer. Certain factors determine the duration of Suboxone withdrawal, including if the medication is gradually tapered down or quit cold turkey.
Suboxone withdrawal generally follows the following timeline:
Day 1-3: Withdrawal symptoms may begin within 6-12 hours since the last Suboxone dose. Early symptoms include anxiety, fatigue, and general discomfort. Suboxone withdrawals may then peak within the first 72 hours and include symptoms such as fever, body aches, nausea, vomiting, and diarrhea.
Days 4-7: Symptoms begin to reduce in intensity and gradually subside within this period. Most of the symptoms subside by the end of the first week. However, individuals may begin to experience some of the psychological symptoms of Suboxone withdrawal, such as anxiety and irritability during this period.
Weeks 2-4: During this period, individuals are more susceptible to psychological withdrawal symptoms such as depression. Symptoms such as anxiety and cravings can also continue long after the acute withdrawal phase.
Months: Depression and cravings are likely to persist after a month. In some cases, opioid cravings can appear years after an individual has stopped using the medication. Therefore, improving relapse prevention skills is crucial to stop individuals from using the medication again.

Suboxone withdrawals generally occur within 24 hours of the last dose, peak within 72 hours, and last for approximately a month. The physical symptoms subside within about a week, while the psychological symptoms such as depression and cravings can linger for longer. However, the severity and duration of Suboxone withdrawal may vary from person to person based on factors such as:
One strategy to lessen the severity of withdrawal symptoms is to taper off Suboxone gradually. If you wish to stop using Suboxone, consult your healthcare practitioner first.
Tapering down Suboxone doses under the guidance of a treatment provider is generally the recommended method to quit Suboxone treatment without experiencing significant withdrawal symptoms. Since the body has been accustomed to functioning with Suboxone over a long period, utilizing a tapering program can help the body gradually adjust to functioning without Suboxone and minimize the severity of withdrawal symptoms.
Some people may experience unpleasant withdrawal symptoms even during a tapering program. During such instances, medical treatment at a Suboxone detox facility is recommended.
In addition to utilizing a tapering down program or medication-assisted detox program, people can also follow these simple day-to-day habits to manage Suboxone withdrawal:
Although the risk of withdrawal when using Suboxone as a MAT treatment is a cause for concern, it’s still an effective treatment choice for helping people with opioid addiction achieve and maintain long-term sobriety.
If you are seeking help with your loved one’s addiction, contact us today or complete our quick contact form below, to speak with an addiction treatment specialist.
If you need help with your substance use disorder, we are here to help you build your confidence and momentum towards the future you want. We provide treatment services for adults with alcohol, opioid, and other substance use disorders. We are currently located in Louisiana, Massachusetts, North Carolina, New Jersey, Ohio, Texas, and Washington.
 What Are Suboxone Strips Used For?
What Are Suboxone Strips Used For?
 Six Questions to Ask When Choosing an Addiction Treatment Program
Six Questions to Ask When Choosing an Addiction Treatment Program
 Benefits of Online Addiction Treatment
Benefits of Online Addiction Treatment