Xylazine, also known as ‘Tranq,’ is a potent sedative that has been showing up in the supply of multiple illegal substances and leading to worse outcomes for users. While it was developed in 1962, it started to infiltrate the heroin/fentanyl supply in the 2000s. It is used as a filler, which reduces the amount of opioids in the product and makes it cheaper to sell. [7]
This powerful central nervous system depressant is chemically similar to the blood pressure medication clonidine. However, unlike clonidine, clinical trials for Xylazine in humans were terminated due to extreme adverse reactions. Thus, it is not intended or approved for humans to use. [1].
The U.S. Food and Drug Administration (FDA) has only approved xylazine for veterinary use, in which it is often used as a sedative, analgesic, and muscle relaxant for animals. It is available in liquid form and is often administered intravenously or intramuscularly in conjunction with other anesthetics, like ketamine or barbiturates, ensuring effective sedation for the animal prior to anesthesia. [2].
Notably, xylazine has not been declared a controlled substance and has not required monitoring when dispensed or sold. While it can be legally purchased for veterinary use, it is often being illegally purchased in both a liquid and powder form without a veterinary license. [2].
Despite ongoing efforts by states and the federal government to classify xylazine as a controlled substance and the FDA’s focus on restricting its importation, it remains readily available and poses a risk of contamination in the opioid supply. [1]
While Xylazine has been in the opioid supply in Puerto Rico for some time, it was discovered in Philadelphia in 2006 and has since become prevalent in the area. It has since spread to other regions with the largest increases in the Northeast and South. [7,]
In addition to being called ‘Tranq’ and ‘Tranq dope’ when mixed with heroin/fentanyl, xylazine has also garnered the nicknames ‘zombie drug,’ ‘sleep cut,’ and ‘Philly dope’. [4].
Operating as a central nervous system depressant, it ushers in drowsiness, amnesia, and a deliberate reduction in necessary functions such as respiration, heart rate, blood sugar and blood pressure descending perilously to minimal levels [6]. Some users find xylazine intensifies and/or prolongs the effects of opioids [2]. However, many others find it leads to blackouts, reducing the chance to feel relief and waking up to a more intense withdrawal. [7].
As a sedative, xylazine can lead to excessive drowsiness. Opioids are also a central nervous system depressant and, when combined with xylazine, can produce a sedative state, creating an environment ripe for crimes like robberies and sexual assaults. [7].
Another painful consequence of having to use opioids laced with xylazine is the outcome of injecting it. Xylazine leaves painful wounds that lead to tissue death, infection, and, for many, amputation. [2] These injuries seem to deteriorate more rapidly compared to other skin wounds and can appear on body parts distant from injection sites. [7, 11]
For many, withdrawal from opioids laced with xylazine can be excruciating. In addition to the intense discomfort of withdrawing from opioids, users endorse additionally experiencing migraines, mood swings, and excruciating anxiety with some developing chest pains, seizures and severe hypertension [2, 7, 11].
Since xylazine is being used in conjunction with opioids, overdoses have become more difficult to reverse. Both substances can induce respiratory depression and the combination increases the risk for fatal overdose. [2].
Opioid overdoses are often reversed with the opioid-blocker naloxone/Narcan®. However, there is no current FDA-approved antidote to xylazine in humans. Overdoses of fentanyl laced with xylazine can be less responsive to naloxone. [2].
Overdoses of fentanyl with and without xylazine can appear the same [11]. If someone appears unresponsive, it is imperative to first call 911. If naloxone is available, it should be administered since it can reverse the effects of the opioid. If the person is still unresponsive, monitor their breathing and protect their airway. If they are not breathing, provide rescue breaths by tilting their head back, pinching their nose and giving 2 breaths into their mouth while waiting for help to arrive. Rolling them onto their side into the recovery position can also be beneficial. [10]
Treatment is available in many forms for xylazine use. It can include accessing a facility that offers wound care, supplies and education about how to avoid infections via safe injection techniques. Swift intervention using basic wound care techniques can prevent infection and escalation to amputation or even death. [11].
Other harm reduction techniques such as carrying naloxone and only using with another person around can be life-saving. Never Use Alone is a nationwide initiative that connects callers to trained responders who can help support and call 911 if the caller becomes unresponsive. Another route to reducing harm is to use test strips that detect xylazine before using. [10].
For withdrawal treatment, prescribers have access to anti-anxiety medications such as benzodiazepines and alternative alpha-2 adrenergic agonists, like clonidine, that can lessen the severity of symptoms. Additionally, opioid withdrawal should be treated as soon as possible to reduce the severity of withdrawal. [11]
For those looking for long term abstinence, treatment is available with inpatient/residential, intensive-outpatient and outpatient levels of care.
Eleanor Health provides comprehensive outpatient addiction treatment for adults struggling with alcohol and substance use disorders. Medication, therapy and recovery counseling are available and can be provided virtually.
We serve Texas, Ohio, North Carolina, Washington, New Jersey, Florida, Louisiana, and Massachusetts. Contact us and join us in building confidence and momentum for the future you envision.
Related Articles
 All About Kratom
All About Kratom
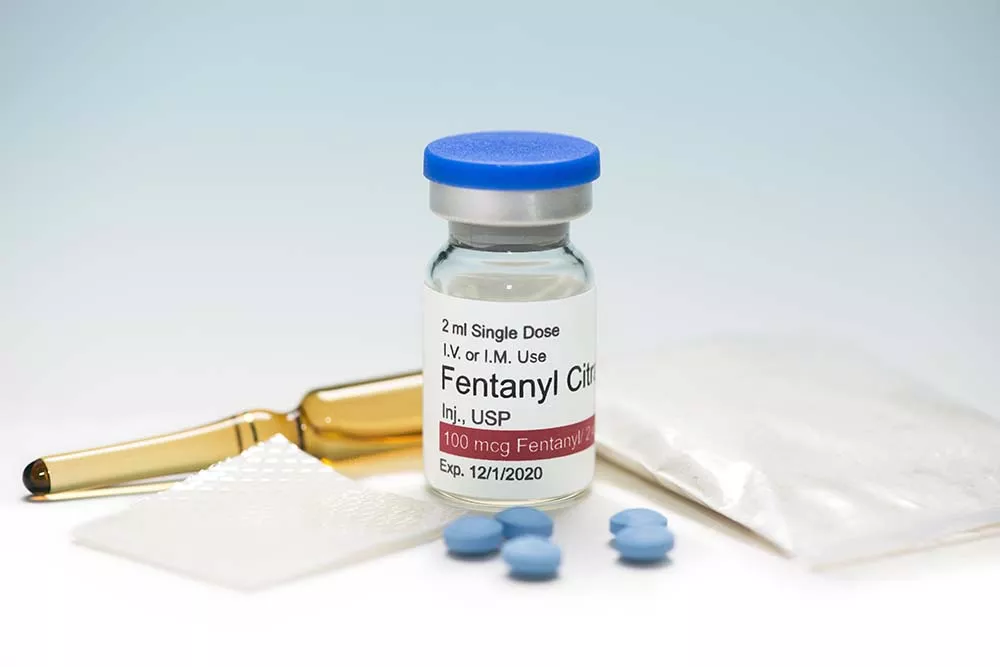 What You Need to Know About Fentanyl
What You Need to Know About Fentanyl
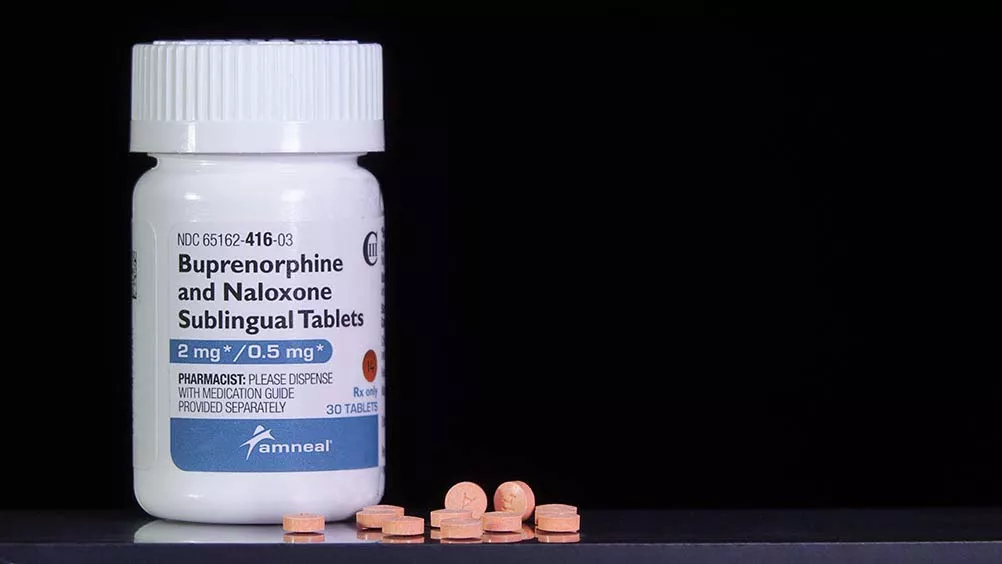 How Long Does Suboxone Stay in Your System?
How Long Does Suboxone Stay in Your System?