Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that affects children and adults. Recent estimates suggest that about 16.13 million adults in the United States (roughly 6.2% of the population) have ADHD, with more than half receiving their diagnosis later in life. For many, this diagnosis provides long-awaited clarity about challenges they’ve faced for years.
Understanding ADHD alongside its common co-occurring conditions is essential for finding the right support. In this blog, we’ll explore symptoms of ADHD, highlight frequent co-occurring mental health conditions, discuss treatment approaches, and share evidence-based strategies to help individuals with ADHD thrive.
ADHD primarily affects executive functioning, the mental skills that help with focus, planning, organization, and self-control. Symptoms fall into two main categories:
Inattention
Hyperactivity and Impulsivity
While everyone experiences moments of distraction or restlessness, people with ADHD face these challenges consistently across different parts of life. The difference lies in how the ADHD brain processes and regulates attention and behavior. For many, this can create daily obstacles at work, in school, and in relationships. But with the right support and strategies, symptoms can be managed effectively.
Accurately recognizing and identifying attention-deficit/hyperactivity disorder takes a well-trained professional. While your primary care physician may be able to make recommendations or refer you to a mental health professional, they are often not trained or qualified to make a diagnosis.
To be diagnosed with ADHD, a person must have experienced several qualifying symptoms frequently and in multiple areas of life (work, relationships, school, etc.) over the last six months. They must also have shown many symptoms in childhood if they’re now an adult. Professionals may also gather information about family history with the disorder since there seems to be a strong genetic component in its development.
If you’ve experienced many ADHD symptoms that have significantly impacted your life, talk to your doctor about your concerns and options. They can help you understand the disorder and refer you to a specialist who can further help.
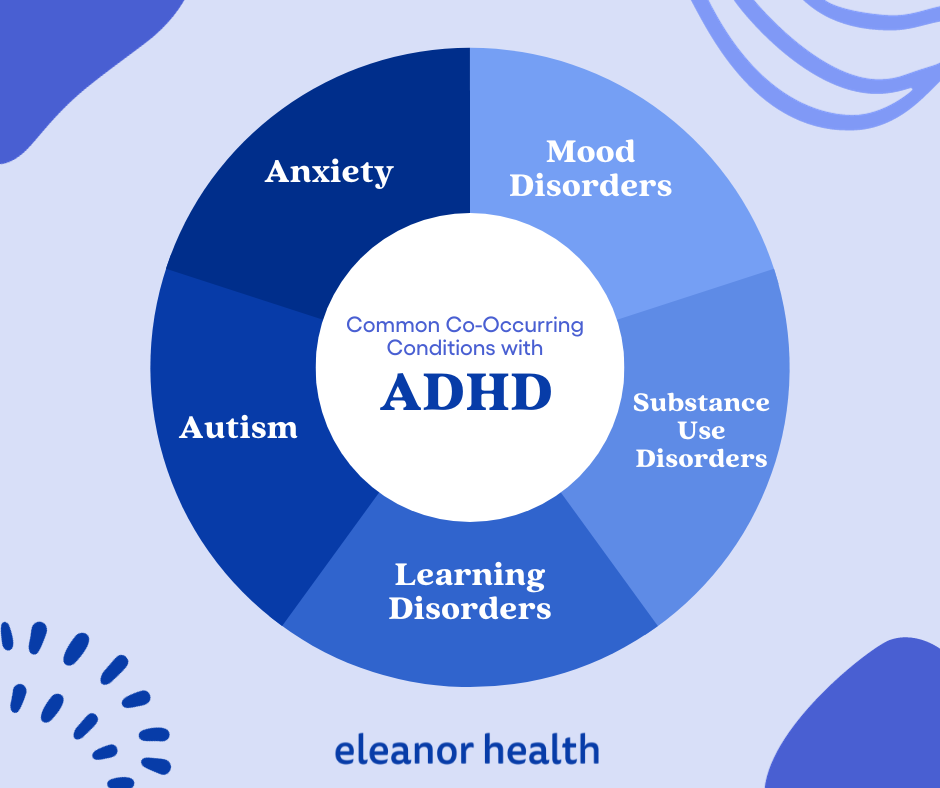
As we stated earlier, many adults with ADHD have at least one or two additional psychiatric conditions. This is known as comorbidity, and it can amplify the symptoms of ADHD or mask them. Recent research shows that over 50% of adults have at least one co-occurring condition, with nearly 40% having multiple conditions.
Anxiety disorders frequently co-occur with ADHD, often leading to more severe symptoms and earlier onset than anxiety alone. Common symptoms like difficulty focusing and restlessness can appear in both conditions, making professional assessment essential. Treatment typically combines medication, psychotherapy, and lifestyle changes, though some ADHD medications may increase anxiety symptoms. Studies show that Adults with ADHD are about 4 times more likely to have generalized anxiety disorder (GAD) compared to those without ADHD.
Individuals with ADHD frequently experience mood disorders like depression or bipolar disorder. The overlap in symptoms (difficulty concentrating, distractibility, impulsivity) can complicate diagnosis. Effective treatment often involves a combination of mood-stabilizing medications and psychotherapy, particularly cognitive behavioral therapy.
Both ADHD and ASD are neurodevelopmental conditions that can share symptoms like difficulty with social interactions and environmental sensitivity. When both conditions are present, treatment plans typically include behavioral therapy, social skills training, and environmental accommodations to help navigate daily challenges.
While ADHD itself isn’t a learning disorder, it frequently co-occurs with specific learning disabilities or challenges. Common learning disabilities include dyslexia, which affects reading ability; dyscalculia, which impacts mathematical understanding; and dysgraphia, which causes difficulties with writing. These combinations of ADHD and learning disorders can significantly impact both academic performance and professional success, often necessitating specialized educational support and various accommodations to help individuals reach their full potential.
Research shows that about 23% of people seeking treatment for substance use disorders also have ADHD. This high overlap occurs for two main reasons: the impulsivity that comes with ADHD can make people more vulnerable to substance abuse, and some people use drugs or alcohol to try to manage their ADHD symptoms on their own. Treatment becomes complex because while ADHD medications can be very helpful, some of them carry a risk of abuse, which must be carefully considered for someone in addiction recovery.
Additional conditions that may co-occur with ADHD include:
These combinations can further complicate diagnosis and management. Managing ADHD with co-occurring conditions requires a comprehensive approach that considers how different conditions interact. Finding the right combination of treatments and support strategies for each individual’s unique situation.
Despite previous thought that it was a disorder to be “outgrown” after childhood, recent research indicates that ADHD is often chronic. While there’s currently no cure, there are many ways to manage symptoms.
Treatment for ADHD often combines medications, therapy, lifestyle strategies, and long-term management.
It’s important to remember that different treatments work better for different people, and finding the most effective plan may require some trial and error. If you or a loved one is experiencing symptoms of ADHD, seeking a medical evaluation is an essential first step. Talk with your doctor about your concerns and available options, as treatment should always be tailored to your unique needs.
When ADHD occurs alongside another mental health condition, treatment must address both together rather than separately. Overlapping symptoms can complicate diagnosis, so a thorough evaluation by a qualified mental health provider is essential.
Effective care often involves:
1. Acknowledge the impacts on a personal, emotional, and social level
The most crucial step in managing ADHD and coexisting conditions is acknowledging the full impact these conditions can have on a person’s life. Taking stock of symptoms and how they are impairing daily or long-term functioning and goals can help clarify what needs improvement. It is also essential to recognize any guilt or self-judgment associated with having both disorders so they can be dealt with head-on.
2. Talk to a mental health specialist
Today, more resources are available than ever to help individuals with ADHD and coexisting conditions deal with their symptoms. Individuals should reach out to a mental health provider to discuss their symptoms and receive a full assessment. In addition, support groups and online forums can help those who struggle with symptoms find additional resources and support.
3. Develop a comprehensive treatment plan
Once diagnoses are made, it is important to work closely with a provider to develop a comprehensive treatment plan. Plans should be personalized and can include non-pharmacological and pharmacological approaches to improving symptoms. Treatment plans that are most successful address all comorbid conditions.
4. Practice self-care
Stress can exacerbate symptoms of ADHD and coexisting conditions, so it is important to practice regular self-care. This could include improving sleep quality, eating a balanced diet, exercising regularly, and engaging in relaxation activities such as yoga or meditation. In addition, you should reduce your exposure to environmental toxins like secondhand smoke and unnecessary stressors like overworking. Finally, tools like mindfulness can improve overall well-being in addition to improving symptoms of almost all mental health conditions.
5. Long-term management
ADHD and comorbid mental health conditions are often chronic, and relapsing symptoms can arise. Continued check-ins with a mental health provider, along with adherence to treatment plans, can reduce the risk for breakthrough symptoms. Keeping track of symptoms and noticing patterns that exacerbate or improve them can also prevent them from occurring.
Living with ADHD and coexisting conditions can be challenging, but it is possible to manage them effectively. Taking note of daily struggles, reaching out to start treatment, developing a plan, making lifestyle adjustments, and putting in the effort over time are the best ways to manage symptoms and achieve success. At Eleanor Health, we specialize in treating adults with Attention-Deficit/Hyperactivity Disorder (ADHD) and comorbid psychiatric conditions, including substance use disorders. More so, we offer compassionate, evidence-based care and strive to improve the quality, delivery, and accessibility of treatment. Contact us today to get started.
 ADHD Symptoms and Treatment
ADHD Symptoms and Treatment
 Therapy for Anxiety, Depression, Trauma: 3 Common Types
Therapy for Anxiety, Depression, Trauma: 3 Common Types
 Natural Treatments for Depression: Can They Help?
Natural Treatments for Depression: Can They Help?